Blog posts
Transforming Clinical Guidelines into Actionable Clinical Decision Support (CDS) Rules
Published on 21 August 2024Managing multimorbidity, especially in elderly patients with mild cognitive impairment (MCI) or mild dementia (MD), presents complex challenges that require sophisticated solutions [1]. The CAREPATH Project stands at the forefront of addressing these complexities by developing an integrated care platform tailored to multimorbid older adults with MCI or MD. The project’s core mission is to empower multidisciplinary care teams to craft personalized care plans while adhering to evidence-based guidelines.
One of the major obstacles in achieving this goal is translating the wealth of information found in clinical guidelines into implementable Clinical Decision Support (CDS) services [2]. These services are crucial for providing real-time, patient-specific recommendations that can help healthcare providers make informed decisions [3]. However, integrating clinical guidelines into practical, actionable tools for healthcare providers is still challenging for many reasons, such as ethical and legal issues, the intellectual challenge of creating knowledge, and technical dimensions [4-5]. At the heart of our approach is a robust methodology designed to bridge the gap between complex clinical guidelines and actionable Clinical Decision Support (CDS) rules. In CAREPATH, we developed an effective methodology to transform detailed clinical guidelines into CDS rules that guide patient care effectively.
Our Methodology: From Guidelines to CDS Rules
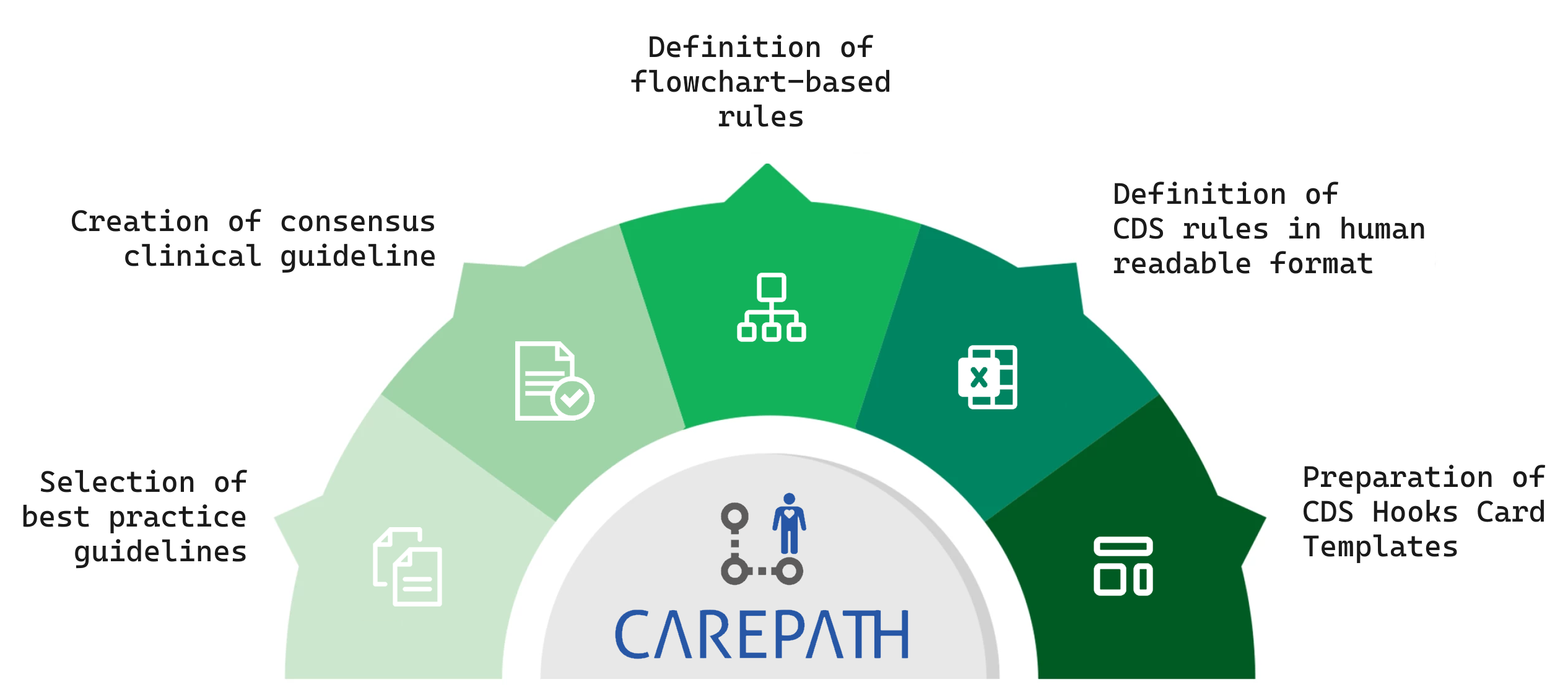
Our methodology involves several key steps to ensure that clinical guidelines are effectively converted into practical CDS rules:
- Guideline Analysis and Breakdown: We start by thoroughly analyzing clinical guidelines from various sources, such as the CAREPATH consensus clinical guidelines. This involves breaking down the guidelines into their core components—recommendations, actions, and conditions—across a range of health issues including hypertension, diabetes, heart failure, and more.
- Flowchart Development: To visualize the decision-making process, we create detailed flowcharts that outline the clinical pathways and decision points specified in the guidelines. These flowcharts serve as a foundational tool for developing CDS rules by mapping out the logical sequence of actions and interventions recommended by the guidelines.
- CDS Rules Definition: Based on the flowcharts, we define CDS rules that capture the essence of the clinical guidelines. Each rule is crafted to address specific aspects of patient care, such as diagnosis, treatment, lifestyle advice, and goal management. For instance, our rules for hypertension management include detailed criteria for diagnosing and categorizing the condition, setting treatment goals, and adjusting medication based on patient-specific parameters.
- CDS-Hooks Specifications: We then translate these rules into implementable CDS-Hooks specifications, which are designed to automate the application of the guidelines within clinical systems. Each CDS-Hook specification is associated with a specific action or recommendation, such as suggesting a follow-up appointment or adjusting medication dosages. These specifications are detailed and implementable, ensuring that they can be integrated into IT systems effectively.
- Implementation and Testing: The CDS rules and CDS-Hooks specifications are implemented using a scalable programming approach, such as Scala for the CAREPATH project. The rules are encoded into FHIR Path expressions and instantiated as CDS Hooks cards, which are then tested for accuracy and functionality within IT systems.
- Integration into Clinical Workflows: Finally, we integrate these CDS services into the Adaptive Integrated Care Platform (AICP). This platform provides a user-friendly interface for healthcare professionals, allowing them to access CDS recommendations seamlessly within their existing workflows. The platform supports the real-time application of guidelines, enhancing decision-making and patient care.
Key Achievements and Insights
A key feature of the CAREPATH methodology is its emphasis on collaboration between clinical experts and software engineers. This interdisciplinary approach ensures that CDS services not only adhere to clinical guidelines but are also technically feasible. By bridging the gap between medical expertise and technical implementation, we enable the creation of CDS solutions that are both practical and effective, enhancing the quality of care for patients with complex health needs. Additionally, the systematic nature of our methodology provides a repeatable framework for transforming clinical guidelines into CDS rules, making it scalable for different guidelines and healthcare contexts. By adhering to standards such as CDS Hooks and HL7 FHIR, our approach facilitates interoperability between different health IT systems, promoting widespread adoption and integration of CDS services.
Future Directions
Our methodology not only addresses the immediate challenge of automating clinical guidelines
but also sets the stage for future advancements. Upcoming studies will evaluate the usability
and effectiveness of our CDS services in real-world settings, providing valuable insights
into their impact on patient care and clinical decision-making.
Through our approach, we aim to make clinical decision support more accessible and effective,
ultimately improving patient outcomes and enhancing the efficiency of healthcare delivery.
You can find further details about this article in our paper, which has been recently published
in the Frontiers in Medicine Journal:
https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2024.1386689/full
References
- Mercer SW, Smith SM, Wyke S, O'Dowd T, Watt GC. Multimorbidity in primary care: developing the research agenda. Fam Pract. (2009) 26:79–80. doi: 10.1093/fampra/cmp020
- Lichtner G, Spies C, Jurth C, Bienert T, Mueller A, Kumpf O, et al. Automated monitoring of adherence to evidenced-based clinical guideline recommendations: design and implementation study. J Med Internet Res. (2023) 25:e41177. doi: 10.2196/41177
- Kruse CS, Ehrbar N. Effects of computerized decision support systems on practitioner performance and patient outcomes: systematic review. JMIR Med Inform. (2020) 8:e17283. doi: 10.2196/17283
- Sutton RT, Pincock D, Baumgart DC, Sadowski DC, Fedorak RN, Kroeker KI. An overview of clinical decision support systems: benefits, risks, and strategies for success. NPJ Digital Med. (2020) 3:17. doi: 10.1038/s41746-020-0221-y
- Mayo AT, Myers CG, Bucuvalas JC, Feng S, Juliano CE. Supporting robust teamwork-bridging technology and organizational science. N Engl J Med. (2023) 388:2019–21. doi: 10.1056/NEJMp2300172
 This project has received funding from the European Union’s
Horizon 2020 research and innovation programme under grant
agreement No 945169
This project has received funding from the European Union’s
Horizon 2020 research and innovation programme under grant
agreement No 945169